In this area you will find a list of common tests which are ordered to help diagnose spine conditions and what each test entails. Click on the links below to review each test in detail. If you have any questions about any test in particular and whether it may be appropriate for you, contact us to schedule an appointment to review it in detail.
X-ray
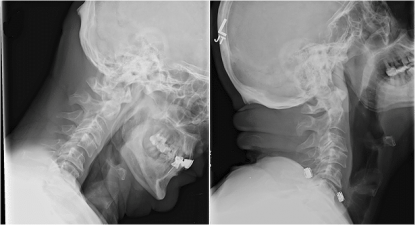
X-rays are a fairly ubiquitous way of imaging the human body. They are used to look for pneumonia’s, broken bones and a number of other issues. X-rays involve passing a beam of electromagnetic radiation through your body. Once the beam passes through your body it strikes a detector which measures the amount of X-rays which were able to pass through and generates an image. In most x-rays, bones will show up as white (see Figure 1) because they are dense and don’t allow the x-ray beams to get through them. On the flip side, things such as your lungs will show up black because they are mostly full of air and allow the x-ray beam to go right through. Other organs will show up in shades of grey depending on how dense they are.
MRI
MRI stands for magnetic resonance imaging. It is one of the best tools for evaluating your spine anatomy in detail and allows your surgeon to see the spinal cord and nerve passageways in detail (see Figure 3). An MRI machine has a large magnet embedded inside of it. You are placed onto a table which slide into the tube of the MRI machine. You may have straps or a face mask to keep your head or body in the appropriate position during the MRI. It’s absolutely critical to remain still for the entire MRI as motion tends to degrade the images. Once the magnet is on, the MRI machine sends and receives radio waves and a computer assembles the output into a detailed image of your spine. One of the downsides to an MRI scan is that it takes longer than most other scans, typically about 30 minutes or so. The plus side is the MRI scan has no radiation associated with it.
MRI’s can be helpful for diagnosing a wide variety of conditions. They are extremely helpful when trying to diagnosis spinal stenosis, herniated discs, spinal tumors, and any other condition causing compression of your spinal cord and nerves. However, as mentioned before the image quality can be affected by a variety of things, including movement during the MRI and/or metal implants in the area around the MRI. Not everyone can have an MRI, including most people with pacemakers, and so expect to fill out a detailed screening form prior to being able to schedule your MRI.

CT or CAT Scan
CT (Computerized Tomogrophy) or CAT (Computerized Axial Tomography) is an imaging technique which takes X-rays from multiple angles and uses a computer to reconstruct multiple images. You’ll lay on a table which slides you into a tube, but unlike the MRI, the CT scan tends to be much quicker and not take as long.
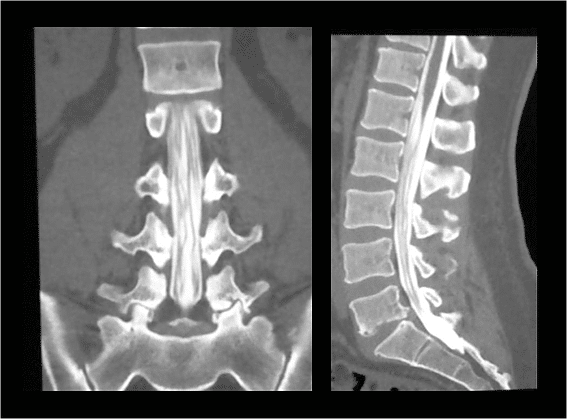
CT scans are typically used to evaluate the anatomy of your bones in more detail than x-rays can show. Other uses for spine surgery include using it as a complement to your MRI (to decide how much of your nerve compression is from bone vs. soft issue), using it for surgical planning (to decide where and what size screws can be inserted into your spine), and for checking to see if attempted spinal fusions have actually successfully fused. CT scans can also be combined with myelograms as a substitute for MRI when someone cannot have an MRI, has too much metal artifact to obtain reasonable MRI images, or for one reason or another is unable to tolerate the MRI scan. The CT myelogram can show the dye injected into the canal and any potential areas of blockage (see Figure 6 for an example of a CT myelogram). The main downside to CT scans are the radiation dose. Unlike MRI’s which are radiation free, CT scans consist of more radiation than just regular X-rays alone. Thus, we only use them when the information they provide will be used to diagnose your condition or change your treatment regimen.

Myelogram
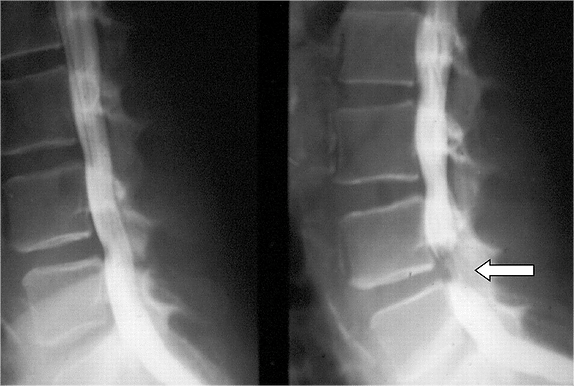
A myelogram involves injecting contrast dye into the sac which contains the nerve roots. This dye then travels up and down the sac and shows up on x-rays taken of your spine. This allows the radiologist and your surgeon to see if there are any areas the dye has trouble making it through which could signify an area of compression around your nerves. On the left panel of Figure 5 is a normal myelogram where the white dye travels up and down the spine without any significant areas of compression. On the right panel of Figure 5 is a myelogram where the dye gets compressed into an hour-glass shape at the level indicated by the arrow. This shows an area of compression on the sac which contains the nerve roots. The myelogram is often combined with a CT scan at the same time which provides much more anatomic detail than a plain myelogram alone (see Figure 6). The dye shows up nicely on the CT scan and can give you high-quality pictures of what’s going on around your nerves. Myelograms are often ordered when MRI’s are unable to be done (ie. due to a pacemaker) or if your spine has a lot of metal implants which degrade the MRI images.
The procedure starts out with you laying on your stomach or side on the x-ray table. The radiologist will use the x-ray to help guide a thin needle into your spinal canal to place the dye into the correct location. After the dye is injected, you’ll have your X-rays taken and if the procedure is being combined with a CT scan you’ll then have the CT done. Because the myelogram involves placing dye into the sac around your nerve roots, there’s always a risk of having nausea or headaches following the scan. Be sure and follow instructions from the radiologist’s office on what to do after your myelogram in terms of activity, drinking plenty of fluids, etc…
Electromyography (EMG) / Nerve Conduction Study (NCS)
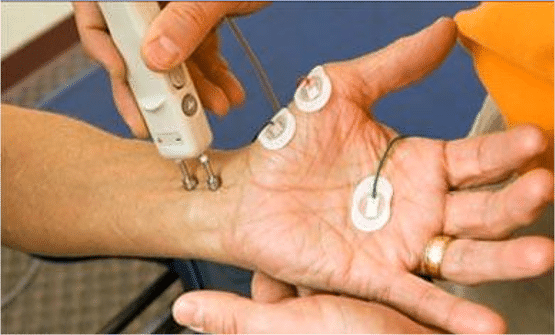
Electromyography (EMG) and Nerve Conduction Study (NCS) are two tests often performed simultaneously to help identify muscle and nerve disorders. Your doctor may order these tests to help identify any associated muscle or nerve dysfunction which could be contributing to your current symptoms. If you already have nerve damage, it can also be used to monitor the progression of your nerve recovery. The EMG portion measures the electrical activity of muscles both at rest and at work. A small needle is placed into the muscle to measure its activity. The Nerve Conduction Study will measure how well the nerves can send and receive electrical signals. It is typically done by placing a stimulator against the skin of your arm and leg. This stimulator then sends a small, brief electrical signal along a nerve. This signal is then picked up by recording electrodes on the skin (see Figure 7 below). By measuring how quickly the signal moves along the nerve, you can get identify portions of the nerve which are diseased and not working normally. Nerve compression can occur anywhere along the path of a nerve from your spinal cord out to your arms and legs. A NCS can help differentiate whether the nerve compression is coming from inside your spine (i.e. from spinal stenosis), outside your spine (i.e. from carpal tunnel syndrome), or a combination of the two.